Features
Don’t panic but flatten the curve
Since I heard a virus could both be an inanimate and living matter at the same time, a keen interest in this phenomenon erupted in me. This can be proven through my first degree in Microbiologist where my final year project was on the Seroprevalence of Hepatitis E virus in a university community which was duly published on Research gate. This came through after spending time in two research laboratories namely Lagos State Drug Quality Control Laboratory and Biosolutions Technologies.
During this great pandemic of COVID-19, a funny but realistic meme ravaged the internet in the Nigerian social media space which says “Graduate of Microbiology that are supposed to be making research on this coronavirus in Nigeria are now Tailors and Make-up Artists”. The immediate notice caused laughter but it was only ephemeral as it questioned my years of studying microbiology in college, then I asked myself what is it can I give at this time if not proper sensitization and awareness about this highly infectious virus amidst diverse rumours.
At the moment , Everyone is out there dishing out different mythological, scientific and religious sentiments about the COVID-19 outbreak as I can vividly recall when the virus was still endemic in China and it had a nomenclature(name) of nCoV (novel-Coronavirus) and the great citadel of learning in West Africa, University of Ibadan, directed two of its entrance examination questions to the virus of which I was a prospective student until I was recommended into the Department of Virology. As at then, None hypothesized that the virus was coming with a greater request which is “Do you really want to know about me?”
Let’s then meet COVID-19.
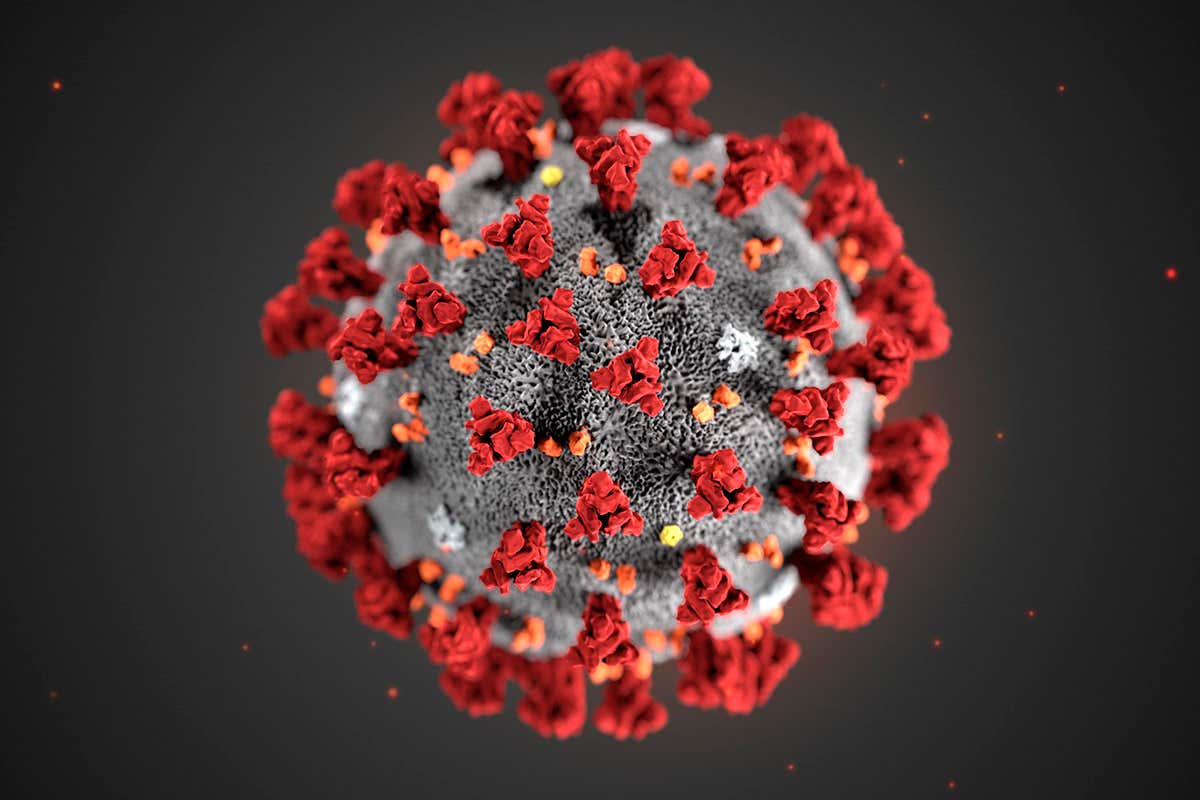
There are actually four coronaviruses that are common in human usually causing moderate respiratory illnesses which are seasonal in nature before the arrival of SARS-COV-2[Severe Acute Respiratory Coronavirus 2], the causative agent of COVID-19[ Coronavirus Disease 2019] as it was fully identified in December 31, 2019 in the province of Wuhan, 2019. SARS-COV-2 is similar to the coronaviruses that circulate naturally in bats due to its 96% genomic similarity before finding it’s way to the human population through an unknown rather yet-to-be identified intermediate host and minimal genetic recombination. In comparison to previously identified coronaviruses, SARS-COV-2 has proven to be more infectious in nature and with aggressive symptoms which can develop to be mild then severe.
According to Worldometers, a renown data source, there are 788,039cases worldwide and 37,877 deaths and 166,411 recoveries with about 5,252 cases in Africa with less than 200 deaths as at the time the article was written. Africa is only posing 0.67% of the World’s total cases which is relevant due to its poor health care system and standard of living. Predictions indicating that the virus is still at its first phase of exponential growth in the continent but this has proven to be meritorious in that it’s has created a form of preparedness by the African leaders before it’s escalates to an uncontrollable level as it has in Europe.
The Science World have definitely relied on the seasonality of flu and flu-like viruses even though that of SARS-COV-2 is yet to be discovered until a pandemic year is fully passed. Taking a closer look at the geographical distribution of the virus, the Chinese neighbours have been able to prevent enormous positive cases due to proactive measures such as early testing and Quarantine as popularly proclaimed a careful observation would reveal that some of them like Singapore is a hot and humid country close to thee equator which must have affected the incessant transmission of the virus also taken a look at South Africa as it already headed into winter which in turn has erratically propagated the transmission of the virus. Cases. The beauty of seasonality is the same reason SARS failed to gain a hold on Africa.
Recommendations and measures from WHO and notable Health parastatals are shouting the effective early testing to curb the spread of the virus. But how do you test for COVID-19? . This can be achieved using three diagnostic methods. Primarily, rRT-PCR ( real-time Reverse Transcriptase Polymerase Chain Reaction) from nasophygneal swab which are highly accurate and can be developed at speed, but they are complex to use and slow to generate results. The other method is through immunoassay which provides historic information about the viral exposure as well as diagnostic evidence. They exploit antibody-antigen recognition either by monoclonal antibodies or cloned viral antigens. It’s usually less accurate, take longer to develop but they are easy to use and deliver result in 20-60 minutes. Unpopularly through CT(Computed Tomography) scan which is useful even before symptoms occur but the American College of Radiology recommends that CT should not be used to screen as a first line to diagnose COVID-19.
South Korea was notably commended on its apt and vital invention of the viral immunoassay kits to save time and sprouts early detection which was necessary because it allows for immediate isolation, contact tracing and the start of supportive treatment. This was required as the infectivity of the virus was so high primarily due to its means and route of transmission. It achieves thus through Person-to-person and contact with contaminated surface which could also be nosocomial(Health workers). For Person-to-person, it’s not air-borne as popularly perceived to be but droplet-borne which is through sneezing and coughing of infected patients would allow the viral suspension in the droplets to get into the close contact respiratory tract and then the replication story continues. For contaminated surfaces, the survival rate of the virus outside a living cell is discovered to be 4 hours on copper material, 24 hours on cardboard and 72 hours on Plastic which explains it’s continued viability in aiding sporadic transmission.
So many persons have been concerned about it’s blood transmission route but the only available information about the virus is it’s replication in the respiratory cells and not in the bloodstream because the blood cells don’t have the receptor cells and binding sites to allow the entry of the virus even though novel publications may prove otherwise but we’re as well safe from it. Another major concern is why close contacts of COVID-19 positives might not be positive to the infection which is primarily due to false negative results of which repetition of the test might be needed or the contact with the positive only occurred when the virus is yet to assemble its various components during replication(avirulent), at this stage it will not be transmissible.
The CFR(Case Fatality Rate) in Italy caused the whole world to panic and dread the arrival of the virus in whatever society which has been identified to be due to situational factors such as aged population, overwhelmed hospitals, shortage of ventilators and lifesaving care rationing not because a more virulent strain has developed in the country.
The only Good news the world is expecting is the arrival of COVID-19 vaccine as various laboratories in the world are already into it’s research. In the midst of the vaccine development, some pessimists have predicted that the virus would likely evolve away from the vaccine but no it won’t. SARS-COV-2 isn’t mutating quickly, suggesting a vaccine would offer lasting protections. Here’s why. The viral genome is only an unsegmented single-stranded RNA unlike the H1N1 swine flu which has 8 segments which takes a pretty weird situation for recombination to occur for a no-segment virus. Secondarily, the genome has a proof-reading machinery that reduces error and pace of mutation. No divergent motion difference has been observed as there are only about 4-10 genetic differences from the original virus in Wuhan so we would be having a single vaccine lasting us for years.
Moreover, here immunity is coming. It requires a large proportion of the population to first get infected, overcome the infection and then maintain sufficient level of antibodies not to get re-infected so the virus can no longer spread and the immunocompromised and immunosuppressed would be protected. The virus can’t overcome herd immunity because of its insignificant mutation differences.
Interestingly, There are no new endogenous infections in China, the epidemic looks to be over because the virus itself will start to slow down owing to some natural factors and know this quote
“For every virus, not every human is equally susceptible”.
To close the curtain, in not panicking our role is to continue the practice of basic hygienic practices such as regular hand washing with soaps at least for 20 seconds, use of hand sanitizers when not close to a water source, Social distancing and Quarantine as Most countries have taken measures at an earlier stage which is our hope and we will know if this is justified in weeks to come. This is the only way you can help flatten the curve and don’t panic.
Written by: Oloruntoba Femi John
BSc Graduate, Department of Microbiology, Federal University Oye-ekiti
Graduate Student, Department of Virology, University of Ibadan
Contact details: +2348130272947
Twitter ID: Oloruntobafemi6
Facebook: Oloruntoba Femi
Instagram: Oloruntoba.femi








Abimbade Mathew Iyanuoluwa
April 2, 2020 at 5:38 am
Waw… Am really exhilarated
Aribisala Dare Oluwatimilehin
April 2, 2020 at 2:12 pm
wow awesome piece
thank you Sir for this insight